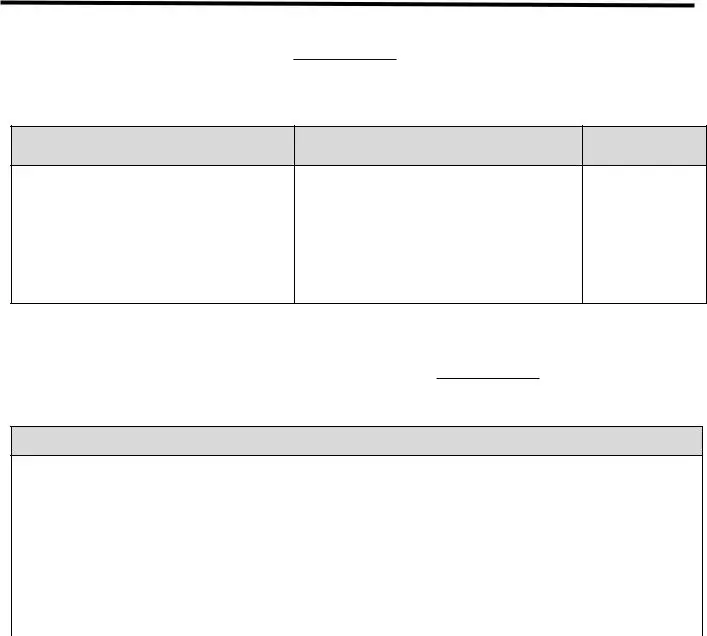
Free Advance Beneficiary Notice of Non-coverage Template
The Advance Beneficiary Notice of Non-coverage (ABN) is a form that informs Medicare beneficiaries when a service or item may not be covered by Medicare. This notice allows beneficiaries to make informed decisions about their healthcare options and potential costs. Understanding the ABN is essential for navigating Medicare services effectively.
Open Editor Now
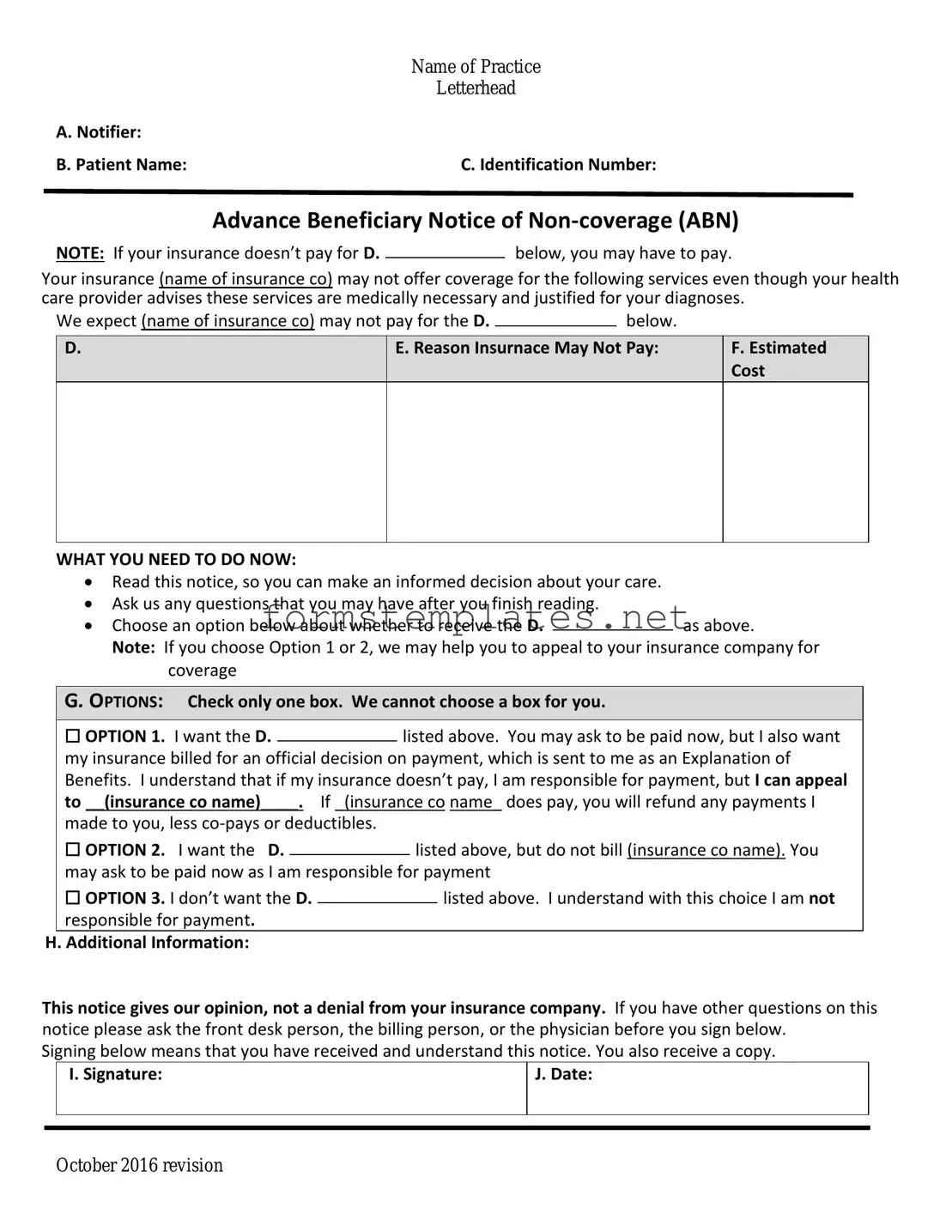
Free Advance Beneficiary Notice of Non-coverage Template
Open Editor Now
Open Editor Now
or
⇓ PDF Form
Your form still needs attention
Finalize Advance Beneficiary Notice of Non-coverage online — simple edits, saving, and download.