Free Tb Test Template
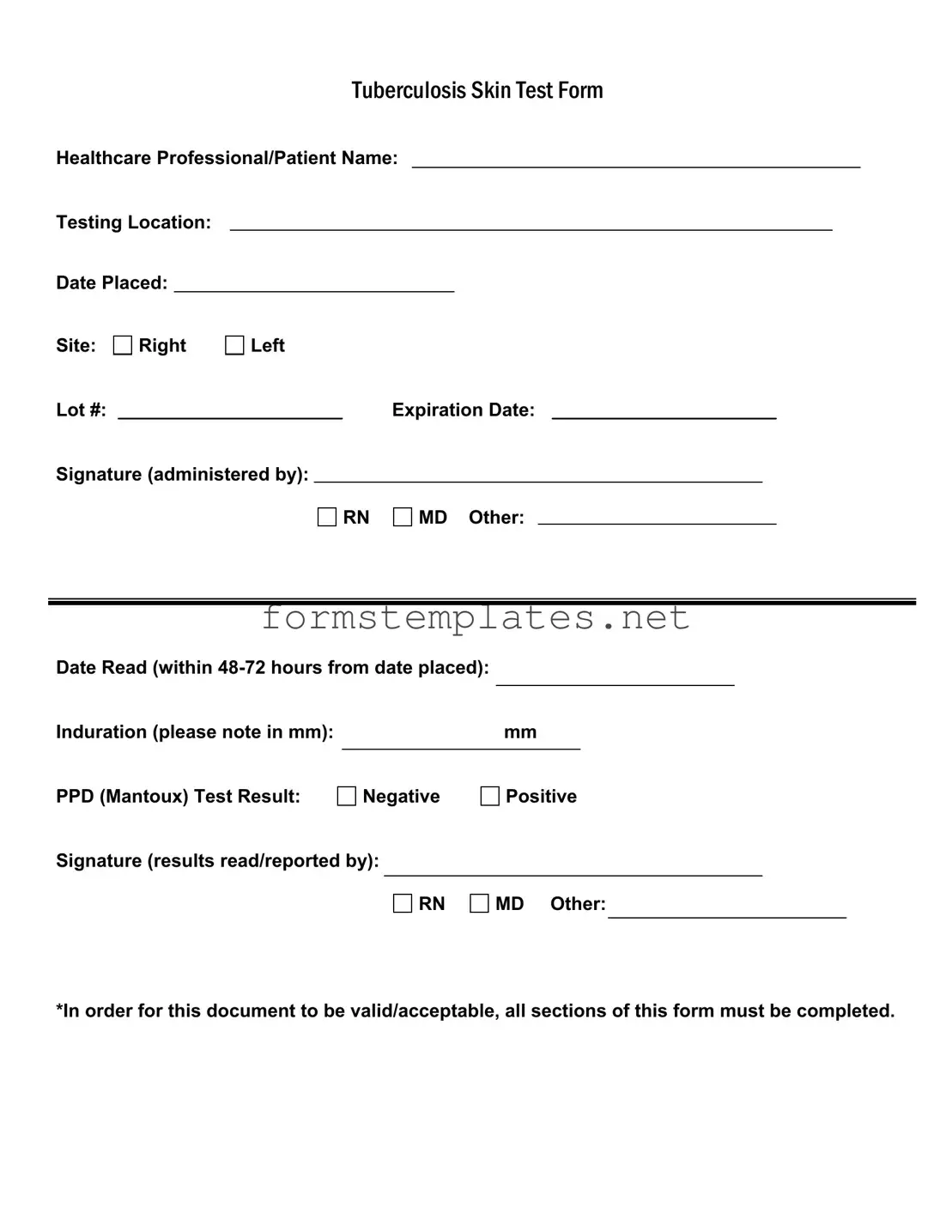
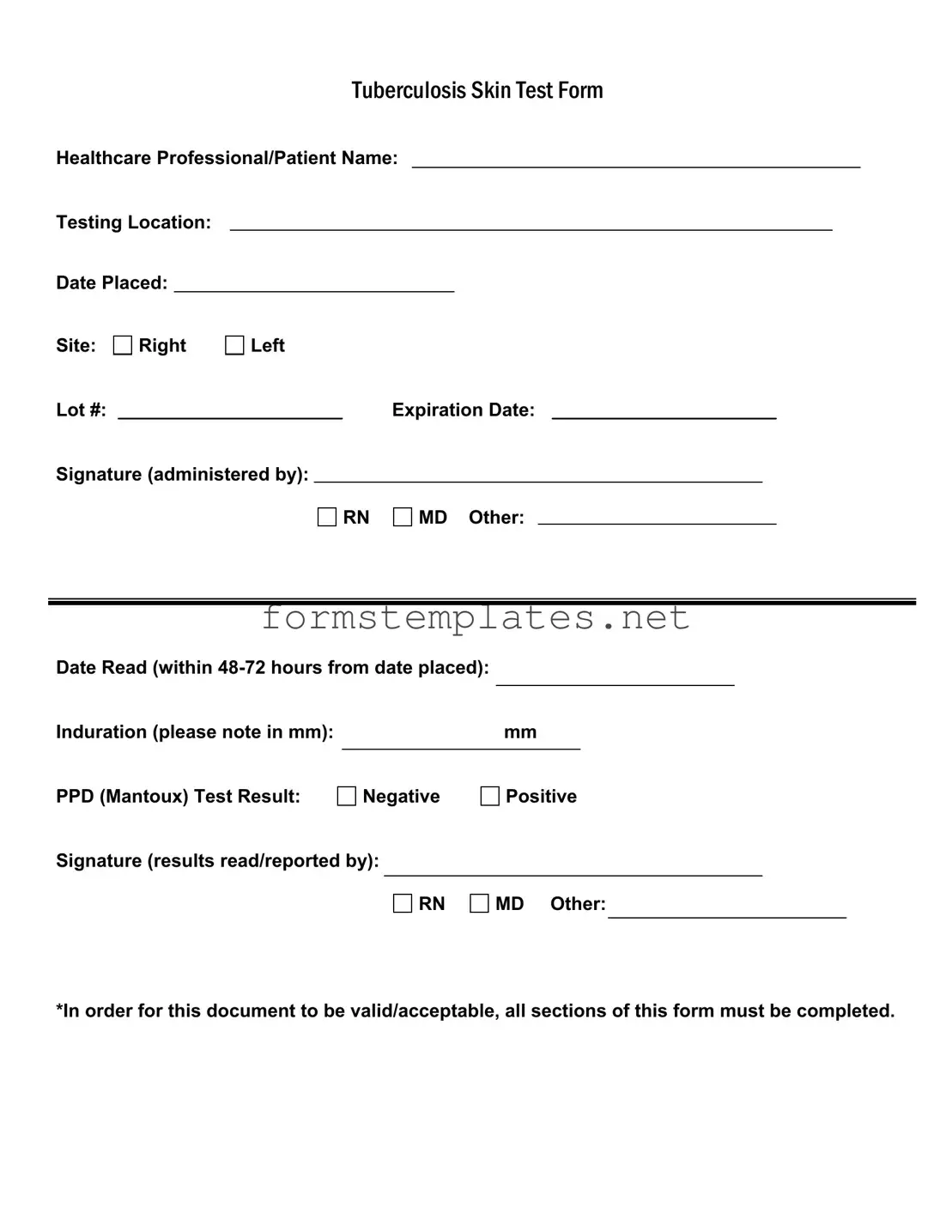
The Tuberculosis Skin Test Form is a critical document used to record the administration and results of the Mantoux test, which helps determine if an individual has been exposed to the tuberculosis bacteria. It includes essential information such as the healthcare professional's name, testing location, and the test results. Proper completion of all sections is necessary for the form to be considered valid and acceptable.
Open Editor Now
Free Tb Test Template
Open Editor Now
Open Editor Now
or
⇓ PDF Form
Your form still needs attention
Finalize Tb Test online — simple edits, saving, and download.